This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.
That cluster of angry red bumps on your neck after yesterday’s shave isn’t just razor burn—it’s folliculitis, a condition affecting millions when bacteria, fungi, or simple friction breach your hair follicles’ protective barriers.
Staphylococcus aureus, the most common bacterial culprit, thrives in warm, moist environments like gym clothes and hot tubs, turning minor irritation into painful pustules within hours.
Whether you’re dealing with barber’s itch from dull razors, hot tub folliculitis from contaminated water, or chronic inflammation from an underlying condition like diabetes, understanding the specific trigger determines which remedy will actually work.
From clinical-grade benzoyl peroxide to properly applied warm compresses, effective treatment targets both the infection and the mechanical factors keeping your follicles inflamed.
Table Of Contents
- Key Takeaways
- What is Hair Follicle Inflammation?
- Common Causes of Hair Follicle Inflammation
- Recognizing Symptoms of Inflamed Hair Follicles
- Diagnosing Hair Follicle Inflammation
- At-Home Remedies for Hair Follicle Inflammation
- Medical Treatments for Severe Folliculitis
- Preventing Future Hair Follicle Inflammation
- Lifestyle Changes for Healthier Hair Follicles
- When to Consult a Dermatologist
- Frequently Asked Questions (FAQs)
- Conclusion
Key Takeaways
- Folliculitis stems from specific bacterial, fungal, or mechanical triggers—identifying whether Staphylococcus aureus, Malassezia yeast, or razor friction drives your inflammation determines which treatment protocol will actually clear your symptoms rather than waste time on ineffective remedies.
- Most mild cases resolve within 7-10 days using targeted at-home interventions like warm compresses, benzoyl peroxide washes, and proper hygiene, but persistent symptoms beyond two weeks, fever, spreading redness, or deep painful nodules signal complications requiring immediate dermatologic evaluation.
- Curly and coarse hair types face elevated risk because tightly coiled strands re-enter skin after shaving while excess sebum clogs follicle openings, making prevention strategies like single-blade razors, loose breathable fabrics, and post-exercise showers critical for breaking recurrence patterns.
- Chronic or severe folliculitis can permanently destroy follicle structures through deep infection and scarring, leaving bald patches or disfigurement—early intervention with appropriate antibacterial, antifungal, or immunomodulatory therapy prevents irreversible damage while addressing underlying conditions like diabetes that compromise skin defenses.
What is Hair Follicle Inflammation?
Hair follicle inflammation, medically termed folliculitis, occurs when the tiny pockets in your skin that anchor each hair strand become irritated or infected. This common dermatologic condition can develop anywhere on your body that grows hair, from your scalp down to your legs, and presents as small red bumps that may resemble acne or heat rash.
Understanding what folliculitis actually is—and why it happens—gives you the foundation to recognize, treat, and prevent this frustrating skin issue.
Building a consistent skincare routine for men helps keep your skin barrier strong and reduces your risk of infection.
Definition of Folliculitis
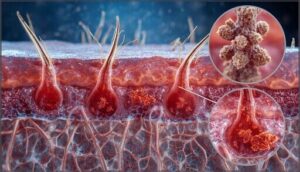
Folliculitis is an inflammation or infection of the hair follicles—the tiny skin pockets where each strand emerges during hair growth.
When bacteria, fungi, or irritants invade follicle structure, you’ll see small red bumps or pustules clustered around individual hairs.
If you notice tenderness, flaking, or hair loss alongside these bumps, check for signs of damaged hair follicles to assess the severity.
This common skin inflammation can strike anywhere hair grows, from your scalp to your legs, manifesting in several folliculitis types depending on the underlying infection causes.
For more details on clinical findings of folliculitis, refer to trusted dermatological sources.
How Hair Follicles Become Inflamed
Your hair follicles become inflamed through several interconnected pathways—microtrauma effects from shaving or tight clothing weaken the skin barrier, creating openings where bacterial infection can take hold.
Once Staphylococcus aureus or other pathogens breach follicle damage sites, your immune system floods the area with inflammatory cells, producing the swollen, red bumps characteristic of folliculitis.
Blocked pores, ingrown hairs, and prolonged moisture further compromise infection control around inflamed hair follicles. Those with curly hair and darker skin types are especially at risk due to specific risk factors for folliculitis.
Areas Commonly Affected
Inflammation shows up where you’d expect—anywhere follicles thrive. Your scalp issues often stem from dense follicle concentration and product buildup, while facial follicles in the beard zone bear the brunt of shaving trauma.
- Scalp: Dense hair follicles meet frequent irritants from styling products
- Face: Bacterial transfer from razors inflames beard and moustache areas
- Armpits: Armpit inflammation follows sweat, moisture, and fabric friction
- Groin: Tight underwear creates groin irritation through constant rubbing
- Legs: Leg bumps emerge from ingrown hairs post-shaving or waxing
Common Causes of Hair Follicle Inflammation
Hair follicle inflammation doesn’t happen randomly—it has specific triggers that you can often identify and address. Understanding what’s causing your folliculitis is the first step toward effective treatment and prevention.
The most common causes fall into four main categories: bacterial infections, fungal and viral triggers, non-infectious irritants like shaving or tight clothing, and underlying risk factors that make your follicles more vulnerable.
Bacterial Infections
When bacteria breach your skin’s defenses through shaving nicks or friction points, they ignite follicle damage that produces those telltale itchy bumps. Staphylococcus aureus ranks as the most common culprit behind bacterial skin infections affecting your follicles, though Pseudomonas aeruginosa from poorly maintained hot tubs can also trigger outbreaks. Both methicillin-sensitive and methicillin-resistant bacterial strains cause similar folliculitis symptoms.
Understanding these bacterial causes helps you take control through proper infection control measures and hygiene practices.
| Bacterial Strain | Common Source | Typical Appearance |
|---|---|---|
| Staphylococcus aureus | Shaving nicks, friction | Small pus-filled bumps, crusting |
| Pseudomonas aeruginosa | Hot tubs, pools | Red bumps on swimsuit areas |
| Gram-negative bacteria | Long-term antibiotic use | Pustules around nose, cheeks |
Fungal and Viral Triggers
Beyond bacterial invaders, yeasts and viruses can hijack your follicles and spark persistent flareups. Malassezia infection thrives in warm, oily environments, creating uniform itchy bumps on your chest and back—often mistaken for regular acne but labeled as fungal acne or yeast overgrowth. Viral outbreaks like herpes simplex produce painful, grouped lesions, while molluscum contagiosum forms dome-shaped bumps.
Here’s how fungal and viral triggers differ:
- Malassezia species multiply in heat and sweat, causing fungal folliculitis that resists standard antibiotics yet clears with antifungal treatment in over 80 percent of cases.
- Dermatophyte infections such as tinea barbae attack beard follicles with painful nodules, broken hairs, and crusting that demand weeks of systemic antifungal tablets.
- Herpes simplex virus creates clusters of burning pustules around your beard, neck, or genital regions, often recurring under stress or sun exposure.
- Molluscum contagiosum and HPV warts spread along shaving lines, especially when you share razors or towels, producing inflamed follicle-centered bumps.
Fungal skin infections and viral skin infections flourish when your immune defenses weaken, sebum production rises, or occlusive clothing traps moisture—making proper diagnosis essential before treatment.
If shaving aggravates already compromised skin, switching to aftershave balms formulated for acne-prone skin can calm inflammation without clogging pores further.
Non-Infectious Irritants (Shaving, Clothing)
Without a single germ in sight, dull razors and tight jeans can torch your skin barrier and ignite hair follicle inflammation through pure mechanical friction.
Even without infection, dull razors and tight clothing can ignite hair follicle inflammation through mechanical friction alone
Shaving techniques that skip lubrication create microtears, triggering razor burn and red bumps along every stroke.
Clothing irritation from synthetic fabrics traps sweat against follicles, while personal hygiene lapses allow oil and debris to block pores—transforming everyday hair care and skin irritation into chronic flareups that friction prevention easily sidesteps.
Risk Factors (Immune Issues, Medical Conditions)
Immune system disorders—whether primary immunodeficiency, autoimmune diseases, or immunosenescence in aging adults—directly weaken your infection prevention defenses, inviting recurrent folliculitis that won’t quit.
Chronic illness like diabetes fuels systemic inflammation, impairing skin health while inflammatory conditions misfire immune responses. Medical conditions that compromise your immunity transform minor follicle irritation into stubborn, treatment-resistant flare-ups demanding dermatologic attention.
Recognizing Symptoms of Inflamed Hair Follicles
You need to know what folliculitis looks like so you can catch it early and respond appropriately.
The clinical presentation varies depending on the underlying cause, infection severity, and your individual skin characteristics. Understanding the range of symptoms—from mild surface irritation to deeper inflammatory changes—helps you distinguish between self-limiting cases and those requiring professional evaluation.
Red Bumps and Pustules
You’ll notice folliculitis symptoms as small, dome-shaped red bumps clustered around individual hair follicles, often topped with white or yellow pus-filled pustules that resemble acne. These lesion types usually appear in crops rather than isolated spots, affecting areas prone to friction like your thighs, back, or beard region.
The pustule formation signals bacterial infection within the follicles, requiring proper follicle care and bump treatment to prevent skin irritation from spreading.
Itching, Burning, and Pain
Your folliculitis symptoms often escalate from visible bumps to intense sensory discomfort, with itching, burning, and pain signaling nerve sensitivity around inflamed hair follicles.
Itch mechanisms involve specialized C fibers carrying inflammatory signals to your brain, while burning sensations arise when mediators sensitize nerve endings. You’ll usually notice tender, sore follicles that worsen with friction, pressure, or heat, distinguishing skin infection from simple skin irritation and guiding appropriate pain management strategies.
Signs of Severe or Chronic Folliculitis
When your inflamed hair follicles won’t settle down after standard care, you’re likely facing deep folliculitis or chronic infection—conditions that demand sharper attention.
Watch for follicle scarring, visible skin lesions that refuse to heal, spreading redness despite treatment, painful abscesses beneath the surface, or patchy hair loss where folliculitis symptoms have destroyed follicles, all signaling that inflammation management requires professional intervention.
Diagnosing Hair Follicle Inflammation
Diagnosing folliculitis usually begins with a straightforward visual examination, though distinguishing it from similar skin conditions requires clinical precision.
You’ll want to know when home observation isn’t enough and medical evaluation becomes necessary. Understanding the diagnostic process, including conditions that mimic folliculitis, helps you take control of your skin health with confidence.
Visual and Physical Examination
Your doctor will conduct a thorough lesion assessment and skin palpation, checking for red bumps, pus-filled blisters, and tenderness around hair follicles. Through careful follicle inspection, they’ll note the distribution pattern and appearance of inflamed hair follicles.
Dermoscopy tools may magnify subtle details, while swabs or skin scrapings help with infection diagnosis when symptoms suggest bacterial or fungal folliculitis.
When to Seek Medical Advice
Most cases of folliculitis respond well to home care within one to two weeks, but certain medical warning signs and skin infection risks demand professional attention. Severe symptom management and emergency care guidelines help you recognize when folliculitis complications require antibiotic treatment or medical consultation for folliculitis.
- Fever above 100.4°F, red streaks radiating from bumps, or rapidly spreading warmth signal systemic infection
- Firm, deeply painful lumps instead of surface pustules suggest boils or abscesses needing drainage
- Symptoms persisting beyond two weeks despite gentle cleansing and warm compresses warrant evaluation
- Widespread rash, facial or groin involvement, or hair loss in affected areas require dermatologist assessment
Conditions Similar to Folliculitis
Several skin conditions mimic folliculitis, making accurate diagnosis critical for effective treatment. Acne vulgaris produces similar red or white-topped bumps but usually includes blackheads and comedones.
Keratosis pilaris creates rough, sandpaper-like bumps on the arms and thighs without pus. Hidradenitis suppurativa causes deep, painful lumps in skin folds, while molluscum contagiosum forms dome-shaped bumps with central dimples.
Prurigo nodularis develops intensely itchy nodules often triggered by chronic scratching.
At-Home Remedies for Hair Follicle Inflammation
Mild folliculitis often responds well to simple at-home care, allowing you to manage symptoms without a prescription.
The key is addressing inflammation early with gentle, targeted approaches that support your skin’s natural healing process. Here are several effective remedies you can start using right away to soothe irritated follicles and speed recovery.
Warm Compresses and Soothing Baths
Heat therapy can disrupt inflammation’s grip on your skin, delivering targeted relief when follicles rebel. A clean washcloth soaked in warm—not hot—water, held against affected areas for 15 to 20 minutes, increases blood flow and softens skin so trapped pus drains naturally.
For broader coverage, consider these follicle care options:
- Saline compress techniques: Add 1 teaspoon table salt per 2-3 cups warm water
- Epsom salt baths: Dissolve magnesium sulfate crystals in comfortably warm water
- Colloidal oatmeal soaks: Calm itching across larger inflamed patches
- Temperature control: Test water on your inner wrist first—target 104-108°F
- Session frequency: Apply compresses 3-4 times daily for mild folliculitis treatment
Always use freshly laundered cloths to avoid reintroducing bacteria, and limit bath time to 10-15 minutes to protect your skin barrier while maximizing skin soothing benefits.
Proper Cleansing and Hygiene
You can reclaim control with gentle skin care that starves bacteria of their breeding ground. Wash folliculitis-prone zones once or twice daily using fragrance-free cleansers or antibacterial soap containing benzoyl peroxide, then pat—never rub—with fresh towels laundered after each use.
This hygiene practice prevents hair follicle infections while shaving techniques like single-blade strokes minimize friction that triggers skin conditions.
Over-the-Counter Treatments
Drugstore shelves offer proven weapons against folliculitis. Benzoyl peroxide washes (five to ten percent) kill Staphylococcus aureus within follicles, while antiseptic soaps and antibacterial soap reduce surface bacteria.
Hydrocortisone cream calms inflammation, topical antibiotics like bacitracin-polymyxin combinations block infection, and soothing lotions with aloe vera gel ease itching—each folliculitis treatment option targeting different mechanisms without requiring a prescription.
Natural Remedies (Aloe, Tea Tree Oil)
You can reach for gentler plant-based allies alongside drugstore products. Aloe vera gel cools inflamed follicles and hydrates irritated skin, while tea tree oil‘s antimicrobial punch fights Staphylococcus aureus when diluted to two to five percent in carrier oil.
These natural antimicrobials and herbal treatments offer skin-soothing support—just patch-test first, since even botanical remedies can trigger sensitivity.
Medical Treatments for Severe Folliculitis
When at-home remedies don’t clear your folliculitis or when symptoms worsen, it’s time to think about prescription treatments that target the specific cause of your inflammation.
Your doctor will determine whether bacteria, fungi, or viruses are behind your symptoms, then prescribe medications designed to eliminate the infection and reduce inflammation. Here’s what you can expect from medical-grade treatments for severe or persistent folliculitis.
Topical and Oral Antibiotics
When bacterial infections drive your folliculitis, you’ll need antibiotic ointments or oral medications to regain control. Topical treatments like mupirocin 2 percent target Staphylococcus aureus directly in affected follicles, while oral options such as doxycycline 100 milligrams twice daily tackle widespread skin infections through your bloodstream.
Using bacterial therapy for the shortest effective duration protects you from antibiotic resistance and clears folliculitis treatment options faster.
Antifungal and Antiviral Medications
When fungal infection or viral infections cause your folliculitis, antifungal medications and antiviral therapy become critical folliculitis treatment options.
Oral fluconazole 150 to 300 milligrams weekly targets Malassezia fungal infections in your hair follicles, while valacyclovir 1 gram twice daily treats herpetic folliculitis caused by herpes simplex. Medication safety matters—your prescriber checks liver function for azole antifungals and screens for drug interactions with existing medications before starting treatment.
Prescription Creams and Lotions
When over-the-counter options don’t clear your folliculitis, prescription formulas step in with targeted power.
Topical antibiotics like mupirocin 2 percent or clindamycin 1 percent gel directly attack Staphylococcus aureus in inflamed follicles, while low-potency steroid creams calm redness short-term.
Your dermatologist may also prescribe emollient lotions to restore your skin barrier, reducing friction that triggers flare-ups, and proper application techniques guarantee you don’t clog follicles with thick layers.
Preventing Future Hair Follicle Inflammation
Preventing folliculitis requires targeted modifications to your daily routines, particularly in activities that repeatedly stress or compromise hair follicles. You’ll need to address three primary risk areas: mechanical hair removal practices, fabric-skin interactions, and exposure to contaminated water or shared personal items.
The following strategies address each category with specific, evidence-based techniques that substantially reduce recurrence rates.
Shaving Techniques and Hair Removal Tips
You can head off hair follicle inflammation by mastering smart shave prep tips and choosing gentler hair removal alternatives. Proper razor selection, careful exfoliation methods, and thorough post shave care dramatically reduce pseudofolliculitis barbae and razor bumps.
- Wash the area with warm water and mild cleanser before shaving to soften hairs and remove bacteria that trigger inflammation.
- Use razors designed for sensitive skin with fewer blades, which decrease tugging and ingrown hairs that inflame follicles.
- Shave in the direction of hair growth rather than against the grain to prevent cut hairs from curling back into skin.
- Apply fragrance-free moisturizer after shaving to restore your skin barrier and protect recently cut follicles.
- Consider laser hair removal or electric trimmers for chronic folliculitis, as these hair removal methods reduce follicle trauma substantially.
Replacing your blade every five to seven shaves keeps cuts clean and minimizes bacterial buildup around vulnerable follicles.
Clothing and Skin Irritation Prevention
Beyond the razor, your wardrobe can defend or damage your follicles. Tight synthetic fabrics trap sweat and bacteria against your skin, fueling inflammation in warm, occluded zones like thighs and groin. Fabric choices, garment fit, moisture management, and laundry practices all determine whether clothing becomes an ally or irritant. Loose cotton or linen garments reduce friction, wick perspiration, and protect vulnerable follicles during exercise and daily wear.
| Prevention Strategy | Skin Care and Hygiene Benefit |
|---|---|
| Choose breathable natural fibers (cotton, linen) | Lowers bacterial overgrowth and sweat accumulation around hair follicles |
| Wear loose-fitting clothing | Reduces friction, pressure, and microabrasions that trigger folliculitis |
| Change out of damp workout gear promptly | Limits prolonged moisture exposure that promotes inflammation |
| Wash exercise clothing after each use with hot water | Removes bacteria, yeast, and skin oils that can reinfect follicles |
Hot Tub and Shared Item Hygiene
Public pools and spas harbor Pseudomonas aeruginosa when chlorine dips below 1 to 3 parts per million, so test strips offer quick infection prevention and control before you soak.
Hot tub folliculitis spreads through contaminated water and shared towels, making personal hygiene practices your strongest defense:
- Shower with soap immediately after soaking to rinse bacteria from follicles
- Never share razors, towels, or swimsuits—even among family
- Wash swimwear after every session to eliminate lingering microbes
Follicle friendly products and hot tub safety habits protect your skin care and hygiene routine.
Lifestyle Changes for Healthier Hair Follicles
Beyond avoiding triggers and practicing careful hygiene, supporting your follicles from the inside out can make a real difference in preventing recurrent inflammation.
Your daily habits—from how you cleanse your skin to how you manage stress and sweat—directly influence follicle health and your body’s ability to fight off bacterial colonization.
Let’s look at three key lifestyle adjustments that can strengthen your skin’s natural defenses and keep folliculitis at bay.
Daily Skin Care Routines
You can take control of folliculitis prevention through a methodical daily routine that keeps follicles clear and calm. Gentle cleansing twice daily with a fragrance-free, non-comedogenic cleanser removes sweat, oil, and bacteria without stripping your skin barrier, while smart moisturizing with lightweight, oil-free formulas maintains skin hydration and reduces irritation.
Incorporating gentle exfoliation tips a few times weekly clears dead cells that block follicle openings, and consistent skin care for folliculitis—combined with proven home remedies for skin infections—substantially lowers your risk of preventing skin irritation and recurring inflammation.
Immune System Support
Strengthening your immune system health creates a foundation for infection prevention and control while reducing folliculitis causes. Support your body’s defenses by prioritizing:
- Nutrient intake of vitamins C, D, zinc, and iron from colorful fruits, vegetables, lean proteins, and whole grains to reduce inflammation control markers
- Sleep patterns of 7–9 hours nightly to stabilize immune-signaling cytokines
- Stress reduction through mindfulness or breathing exercises to prevent cortisol-driven immune suppression
- Microbiome balance with fiber-rich foods that reinforce skin barrier function and prevent skin irritation
Managing Sweating and Oil Production
Sweating and sebum overproduction create an ideal microenvironment for bacterial proliferation within hair follicles, amplifying folliculitis causes and hair follicle inflammation.
You’ll achieve skin balance through sweat reduction strategies—antiperspirants containing aluminum chloride, breathable fabrics, post-exercise showers—and oil control hygiene practices using benzoyl peroxide cleansers, lightweight moisturizers, and gentle exfoliation.
Moisture management prevents the warm, occlusive conditions that trigger hair follicle irritation and inflammatory diseases.
When to Consult a Dermatologist
Most cases of folliculitis respond well to at-home care within a few days to a week, but persistent inflammation signals a need for professional evaluation.
Recognizing when self-treatment isn’t enough can prevent complications like scarring, permanent hair loss, or spreading infection. You should consult a dermatologist if you notice certain warning signs that indicate your folliculitis requires medical intervention.
Persistent or Worsening Symptoms
When folliculitis lingers beyond two weeks despite careful home care, or when red bumps multiply and merge into painful nodules, you’re looking at chronic inflammation that demands medical attention.
Infection spread beyond the follicles, marked by fever, increasing pain, or foul-smelling pus, signals complications of untreated folliculitis. Recurrence patterns, follicle damage, and skin scarring often follow persistent cases, making early dermatologist intervention vital for managing folliculitis symptoms effectively.
Signs of Complications
Red streaks radiating from inflamed follicles, fever above 100.4°F, or a painful lump filling with pus all point to complications of untreated folliculitis that demand urgent care. Watch for these warning signs:
- Abscess formation or boils expanding beyond 2 centimeters, especially carbuncles connecting multiple follicles
- Systemic infection with chills, confusion, or rapid heart rate
- Permanent hair loss and skin scarring from follicle damage on your scalp
Don’t wait—these symptoms need immediate medical evaluation.
Personalized Treatment Plans
Your dermatologist builds a care plan around your specific triggers, symptoms of folliculitis, and lifestyle—not a generic protocol. Here’s how tailored therapy targets your hair follicle inflammation:
| Plan Component | What It Involves | Example Options |
|---|---|---|
| Cause-Targeted Medication | Bacterial, fungal, or irritation-driven infection control | Oral doxycycline, topical mupirocin, antifungal shampoos |
| Daily Skin Care Plans | Personal hygiene practices and product choices | Antibacterial washes, noncomedogenic moisturizers, gentle exfoliation |
| Lifestyle Modifications | Shaving habits, clothing friction, hot tub use | Clippers instead of razors, breathable fabrics, post-workout showers |
| Monitoring Schedule | Treatment outcomes and symptom tracking | Two-week check-ins, flare-up diaries, escalation triggers |
Treatment and management of folliculitis succeed when treatment options match your body’s unique response patterns.
Frequently Asked Questions (FAQs)
Can diet changes help reduce folliculitis outbreaks?
Your skin’s microbiome thrives on what you eat—anti-inflammatory diets rich in omega-3s, probiotics, and proper hydration tips may reduce folliculitis outbreaks by supporting immune function and maintaining nutrient balance around hair follicles.
Is folliculitis contagious through direct skin contact?
Yes, certain types can spread through direct skin contact, particularly when lesions contain Staphylococcus aureus.
Sharing razors, towels, or touching active pustules transfers bacteria between individuals, though proper hygiene substantially reduces transmission risk.
How long does folliculitis typically take to heal?
Most mild cases clear within seven to ten days with basic self-care, though persistent bacterial or fungal folliculitis may require prescription treatment and extend recovery to several weeks before your skin fully heals.
Can folliculitis cause permanent scarring or hair loss?
Deep infections can destroy follicle structures, leaving permanent scars or bald patches, especially with chronic variants like folliculitis decalvans.
Early infection control and avoiding picking reduce follicle damage and support skin regeneration.
Are certain hair types more prone to folliculitis?
Curly, coarse, and oily hair textures carry higher folliculitis risk because tightly coiled strands re-enter the skin after shaving, thick hairs trap beneath the surface, and excess sebum clogs follicle openings, fueling bacterial overgrowth and chronic inflammation.
Conclusion
Persistent discomfort in your follicles doesn’t have to dictate your daily routine. Identifying your specific triggers—whether bacterial colonization, mechanical irritation, or underlying immune dysfunction—determines which hair follicle inflammation remedies will restore barrier integrity.
Most cases respond to consistent hygiene protocols and targeted over-the-counter treatments, though recurrent symptoms warrant dermatologic evaluation to exclude systemic conditions like diabetes or immunosuppression. Your skin’s protective architecture deserves the same diagnostic precision you’d demand for any other organ system.
- https://www.healthline.com/health/skin/folliculitis-home-treatment
- https://www.clnwash.com/blogs/blog/how-do-i-get-rid-of-my-folliculitis
- https://www.medicalnewstoday.com/articles/scalp-folliculitis
- https://www.mayoclinic.org/diseases-conditions/folliculitis/diagnosis-treatment/drc-20361662
- https://averraglow.com/blogs/news/folliculitis