This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.
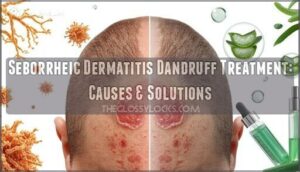
That stubborn white flaking on your scalp isn’t always simple dandruff—and if medicated shampoos barely make a dent, you’re likely dealing with seborrheic dermatitis. This inflammatory skin condition affects nearly 5% of adults, triggered by an overgrowth of naturally occurring yeast that your skin suddenly can’t tolerate.
The result is persistent greasy scales, redness, and itching that refuses to quit. Unlike ordinary dandruff, seborrheic dermatitis often spreads beyond your scalp to your eyebrows, ears, and face, demanding a more strategic approach.
The good news: once you understand what’s driving the inflammation, you can select targeted treatments that actually work and keep flares under control for the long term.
Table Of Contents
- Key Takeaways
- What is Seborrheic Dermatitis Dandruff?
- Causes of Seborrheic Dermatitis Dandruff
- Identifying Symptoms and Signs
- Risk Factors and Triggers
- Diagnosing Seborrheic Dermatitis Dandruff
- Over-the-Counter Treatment Options
- Prescription Treatments for Severe Cases
- At-Home Care and Daily Management
- Long-Term Prevention and Maintenance
- When to Consult a Dermatologist
- Frequently Asked Questions (FAQs)
- Conclusion
Key Takeaways
- Seborrheic dermatitis is a chronic inflammatory condition driven by Malassezia yeast overgrowth that causes greasy, yellowish scales and redness extending beyond the scalp to eyebrows, ears, and face—requiring antifungal treatment rather than standard dandruff shampoos alone.
- Medicated shampoos containing ketoconazole, zinc pyrithione, or selenium sulfide used two to three times weekly form the foundation of treatment by directly targeting fungal overgrowth and reducing inflammation by up to 60%.
- Effective long-term control depends on identifying personal triggers like stress, climate changes, and harsh hair products while maintaining consistent use of antifungal treatments even after symptoms clear to prevent flare recurrence.
- You should consult a dermatologist if over-the-counter treatments fail after four weeks, symptoms worsen with signs of infection like pus or fever, or you need prescription-strength antifungals and calcineurin inhibitors for severe cases.
What is Seborrheic Dermatitis Dandruff?
Seborrheic dermatitis is a chronic inflammatory skin condition that affects areas where oil glands are most active, particularly your scalp. While it shares some features with common dandruff, it’s a distinct medical condition that causes more persistent flaking, redness, and irritation.
Understanding what sets this condition apart will help you recognize it and choose the right approach to managing your symptoms.
Key Characteristics
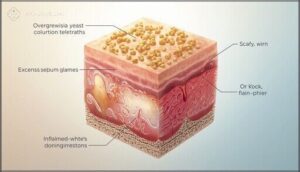
Seborrheic dermatitis appears as oily, irregular patches on the scalp, accompanied by white or yellowish flakes that don’t adhere well. Unlike ordinary dandruff, this condition presents greasy patches rather than dry flakes.
The condition causes itchy skin with varying intensity, and the flakes often accumulate around the hairline and behind the ears. Malassezia yeast is implicated in this persistent scalp scaling.
How It Differs From Regular Dandruff
Regular dandruff involves simple dry flaking without persistent skin inflammation, while seborrheic dermatitis presents with inflamed, reddened patches and greasy yellow scales. You’ll notice seborrheic symptoms extend beyond your scalp to eyebrows, nasolabial folds, and behind your ears—areas regular dandruff rarely affects.
This inflammatory scalp condition responds better to antifungal dermatitis treatment than standard dandruff shampoos alone.
Commonly Affected Areas
Your scalp hosts the condition more than 90% of the time, but seborrheic dermatitis doesn’t stop there. You’ll often see facial symptoms around your eyebrows, nose sides, and nasolabial folds where oil concentrates. Salicylic acid shampoos deliver a proven oily scalp treatment that reduces excess oil by up to 55% in clinical studies.
The area behind your ears and chest can develop itchy skin lesions too.
In babies, trunk eruptions sometimes extend from cradle cap to neck folds in persistent skin conditions.
Causes of Seborrheic Dermatitis Dandruff
You can’t fix seborrheic dermatitis dandruff without understanding what triggers it in the first place. The truth is, multiple factors work together to create those stubborn flakes and irritation on your scalp. These greasy flakes differ from dry scalp symptoms, which produce smaller, drier particles without the accompanying oiliness.
Stubborn scalp flakes don’t come from one cause—multiple triggers work together to create seborrheic dermatitis
Let’s break down the three main causes that dermatologists see most often. If you notice any of these warning signs, explore common scalp conditions linked to hair loss or consult a dermatologist right away.
Role of Malassezia Yeast
You mightn’t realize it, but a tiny yeast called Malassezia lives on your scalp right now. When it overgrows, it disrupts your skin barrier and triggers an immune response that leads to seborrheic dermatitis. Here’s how this fungal growth causes trouble:
- Malassezia feeds on sebum-rich areas
- It releases irritating fatty acids
- Your skin becomes inflamed and itchy
- White or yellow flakes appear
- Microbiome balance shifts dramatically
Antifungal treatments target this yeast infection directly, which is why they work so well for dandruff relief.
Hormonal and Genetic Factors
Your body’s internal signals—androgen influence and genetic testing markers—can shape dermatitis symptoms more than you’d think. Hormone therapy may alter sebaceous regulation, affecting oil production on your scalp. Hormonal shifts can intensify scalp sensitivity, making understanding hair pain triggers essential for effective dermatitis management.
Epigenetic modifications and inherited traits interact to determine if you’ll develop this skin condition. While not a typical fungal infection trigger, these factors influence how your immune system disorders respond to seborrheic dermatitis flares.
Immune System Influences
Your immune response plays a bigger role in seborrheic dermatitis than you might expect. When your skin barrier function weakens, inflammatory pathways activate and worsen flaking.
- Immune system disorders can trigger proinflammatory cytokine release that amplifies symptoms
- Microbiome role on your scalp influences how T cells react to Malassezia
- Inflammatory response intensity varies based on your immune system’s regulation
- Immunosuppression effects may change how your body manages fungal infections
- Altered immune signaling affects both itch and flake formation in susceptible individuals
Identifying Symptoms and Signs
Recognizing seborrheic dermatitis early can help you manage it before symptoms worsen. The signs often start subtle but become more noticeable during flare-ups, affecting how your skin looks and feels.
Understanding what to watch for on your scalp and other areas makes it easier to take action and find relief.
Scalp Flaking and Itchiness
You’ll likely notice greasy, white or yellowish flakes settling on your shoulders—a telltale sign of seborrheic dermatitis dandruff. The itchy scalp that comes with it ranges from mildly annoying to intensely uncomfortable, often worsening during flares.
This itch-scratch cycle makes scalp flaking worse, so effective flake removal and inflammation management are essential for restoring scalp health and improving your overall hair care routine.
Redness and Irritation
Inflamed patches often appear as red, irritated zones on your scalp—evidence that skin inflammation and a compromised skin barrier are at work. Redness grading ranges from mild to severe, correlating with how intense your itchy skin feels.
Irritation triggers like harsh products and UV exposure increase inflammation causes, worsening erythema.
Treating this inflammatory skin condition early helps calm skin reactions and restore comfort.
Symptoms Beyond The Scalp
Seborrheic dermatitis doesn’t confine itself to your scalp—this inflammatory skin condition spreads to other sebaceous-rich zones, creating visible skin health issues that affect your confidence and comfort.
- Facial redness emerges around your eyebrows, nose creases, and behind your ears as oily, scaly patches
- Ear crusting develops along the external canal, occasionally trapping discharge
- Eyelid flaking mimics blepharitis with mild margin irritation
- Chest involvement produces greasy scales on your upper back
- Groin symptoms appear as well-demarcated, oily dermatitis symptoms in rare cases
Risk Factors and Triggers
Some people are more likely to develop seborrheic dermatitis than others, and certain factors can make your symptoms flare up without warning. Understanding what puts you at higher risk helps you recognize patterns and take steps to protect your skin.
Let’s look at the medical conditions and everyday triggers that may be working against you.
Medical Conditions Increasing Risk
Certain underlying health challenges can tip the scales toward more persistent or severe seborrheic dermatitis. When your immune system is compromised—whether by HIV impact, primary immune disorders, or immunosuppressive therapy—your scalp’s defenses weaken, allowing inflammatory skin conditions to flourish. Parkinson’s effects also play a role, as autonomic changes linked to the disease alter skin function and oil production. Understanding these dermatitis risk factors helps you and your provider tailor treatment strategies that address both your skin health issues and chronic infections, giving you real control over flare-ups.
| Condition | How It Affects Seborrheic Dermatitis |
|---|---|
| HIV/AIDS | Increases prevalence and scalp involvement |
| Parkinson Disease | Triggers more persistent, severe flares |
| Immunodeficiency | Weakens skin’s ability to fight yeast overgrowth |
| Immunosuppressive Drugs | Dampens immune response, prolonging symptoms |
Environmental and Lifestyle Triggers
Beyond medical conditions, your day-to-day world shapes seborrheic dermatitis behavior. Climate effects matter—cold, dry winters and humid summers can both worsen flare-ups. Stress management becomes essential, as tension and poor sleep patterns weaken skin defenses and fuel inflammation.
Dietary influences remain under study, but deficiencies in zinc or B vitamins may undermine your skin condition management efforts.
Your skincare routines count too: harsh detergents, heavy oils, and infrequent shampooing create an environment where yeast thrives. Recognizing these dermatitis risk factors puts real power in your hands for daily dandruff and skin care control.
Diagnosing Seborrheic Dermatitis Dandruff
Most cases of seborrheic dermatitis can be diagnosed through a straightforward visual examination by your healthcare provider. Your doctor will evaluate the appearance and location of your symptoms, then rule out other conditions that can look similar on the scalp and skin.
Knowing when to seek professional evaluation and what the diagnostic process involves helps you take control of persistent flaking and irritation.
Clinical Evaluation Process
Your doctor will begin with a dermatologic examination of your scalp, assessing for flaking, redness, and oiliness that match the diagnostic criteria for seborrheic dermatitis.
If there’s any doubt about dermatological conditions like psoriasis or fungal infections, skin scraping or fungal culture may be needed.
This evaluation guides seborrheic dermatitis diagnosis and treatment, ensuring you get the right approach for your specific condition.
Differential Diagnosis
Once your doctor has examined your scalp, they’ll consider other dermatological conditions that mimic seborrheic dermatitis. Psoriasis symptoms like silvery plaques, fungal infections with broken hairs, and contact dermatitis from irritants can all look similar. In unclear cases, a skin biopsy helps confirm the diagnosis and treatment plan.
- Psoriasis can disguise itself with thick, well-defined plaques that demand attention
- Fungal infections steal your hair’s strength, leaving patchy gaps and black dots behind
- Contact dermatitis betrays recent exposures, revealing what touched your vulnerable scalp
- Lichen planopilaris threatens permanent loss, scarring follicles you can’t regenerate
- Atopic dermatitis spreads its reach, intensifying itch across flexural areas you can’t ignore
When to Seek Medical Advice
You should schedule a doctor consultation if over-the-counter dandruff treatments fail after four weeks. Severe symptoms like rapid scalp redness, swelling, or pain warrant immediate attention, especially with fever response indicating infection signs.
Crusting, oozing, or widespread facial dermatitis signal a medical emergency requiring professional skin condition management. Those with immunosuppression need prompt medical research and treatment for new or worsening seborrheic dermatitis symptoms.
Over-the-Counter Treatment Options
Most mild to moderate seborrheic dermatitis cases respond well to treatments you can pick up at your local pharmacy without a prescription. These over-the-counter options target the yeast overgrowth, reduce inflammation, and help remove stubborn flakes that make the condition so frustrating.
Let’s look at the three main categories of products that can give you real relief.
Medicated Shampoos (Zinc, Selenium, Tar)
Zinc pyrithione, selenium sulfide, and coal tar shampoos are front-line treatment options for seborrheic dermatitis, each targeting scalp health through different mechanisms. Zinc and selenium sulfide act as antifungal agents, reducing Malassezia yeast by up to 60%, while coal tar slows skin cell turnover.
These medicated shampoos for dandruff treatment require consistent use—usually two to three times weekly—to control scalp fungal infections and maintain results.
Keratolytic Agents for Flake Removal
Salicylic acid and urea-based products deliver keratolytic effects that soften and dissolve stubborn flakes, making scalp treatment more effective. These keratolytic agents work by breaking down keratin bonds in dead skin, promoting flake removal without harsh scrubbing.
Apply anti-dandruff shampoos with keratolytics two to three times weekly, leaving them on for three to five minutes before rinsing thoroughly.
Safe Use of Topical Corticosteroids
When using topical corticosteroids for seborrheic dermatitis treatment, you’ll want to apply the lowest effective strength for the shortest duration possible to minimize adverse effects like skin thinning.
Follow your healthcare provider’s dosage guidelines carefully, monitoring for stretch marks or worsening redness during corticosteroid therapy. Avoid applying these products to broken skin unless specifically directed.
Prescription Treatments for Severe Cases
When over-the-counter treatments aren’t enough to control your symptoms, your doctor can prescribe stronger medications to break the cycle of inflammation and flaking.
These prescription options target the underlying causes more aggressively and are usually reserved for moderate to severe cases that haven’t responded to standard care.
Let’s look at the three main prescription approaches your dermatologist might recommend.
Topical Antifungal Medications
When over-the-counter dandruff treatment isn’t cutting it, prescription antifungal agents target the skin fungus driving your flare-ups. Ketoconazole 2% shampoo or cream fights Malassezia directly, while clotrimazole 1% lotion addresses fungal infection on affected areas.
For stubborn cases, sertaconazole 2% cream or even oral fluconazole may boost treatment efficacy, though medication resistance occasionally requires adjusting your seborrheic dermatitis treatment plan.
Calcineurin Inhibitors
When standard antifungal agents don’t quiet inflammation, calcineurin inhibitors offer a steroid-sparing alternative for seborrheic dermatitis. Tacrolimus 0.03–0.1% and pimecrolimus 1% work through a unique inhibitor mechanism that blocks T-cell activation, delivering anti-inflammatory effects without the thinning risks of long-term topical applications.
Consider these treatment outcomes:
- Reduced lesion severity in facial and eyelid dermatitis
- Minimal drug interactions or systemic absorption
- Effective dermatology option for corticosteroid-resistant dandruff
Short-Term Corticosteroid Use
When inflammation flares out of control, short-term corticosteroids can bring your scalp back from the brink. Mid- to high-potency topical applications deliver rapid relief for 1–2 weeks, targeting skin inflammation without the long-haul risks of thinning or rebound flares. Your dermatologist will match steroid potency to your seborrheic dermatitis severity, ensuring treatment duration stays minimal while corticosteroid safety remains paramount.
| Potency Level | Typical Duration | Key Dermatological Risks |
|---|---|---|
| Low-Medium | 1–2 weeks | Minimal irritation |
| High | Up to 2 weeks | Skin thinning, telangiectasia |
| Long-term use | Not recommended | Rebound flares, systemic absorption |
Pair corticosteroids with antifungal shampoos to shorten exposure and shift smoothly into maintenance dandruff control—dermatitis management that respects your skin’s limits.
At-Home Care and Daily Management
Managing seborrheic dermatitis doesn’t end with choosing the right product—it requires consistent daily habits that keep flakes and inflammation under control. The way you wash your hair and the adjustments you make to your routine can be just as important as the medication itself.
Here’s what you need to focus on to keep symptoms at bay between treatments.
Shampooing Frequency and Technique
You’ll want to wash your scalp daily or every other day when seborrheic dermatitis flares—weekly shampooing won’t cut it for moderate to severe cases. Your routine matters just as much as frequency:
- Pre-wet thoroughly and apply medicated shampoo with gentle scalp massage to boost circulation without scratching.
- Leave it on for 2 to 5 minutes for maximum flake removal, then rinse completely with warm (not hot) water.
- Pat dry gently to avoid friction that worsens irritation.
Alternating between antifungal and keratolytic formulas maximizes dandruff control while supporting long-term scalp health.
Lifestyle Adjustments for Flare Prevention
Beyond shampooing, small lifestyle adjustments can keep seborrheic dermatitis in check. Stress management and sleep quality both influence inflammation, so finding ways to unwind matters more than you’d think. Scalp hydration with non-irritating moisturizers bolsters your skin barrier, while gentle brushing prevents mechanical irritation when flakes appear.
| Hair Care Tips | Skin Care Tips | Daily Habits |
|---|---|---|
| Avoid heavy oils | Use breathable fabrics | Track flare patterns |
| Rotate medicated shampoos | Apply non-fragranced products | Manage stress levels |
| Limit styling heat | Moisturize gently | Prioritize sleep quality |
| Rinse with warm water | Protect from sun | Support probiotic balance |
These scalp health strategies work best when combined with your treatment plan.
Long-Term Prevention and Maintenance
Managing seborrheic dermatitis doesn’t end when your flare clears—it requires consistent habits to keep symptoms at bay. The right maintenance approach reduces how often flares return and how severe they become when they do.
Three essential strategies form the foundation of long-term control: regular use of targeted treatments, identifying what sets off your symptoms, and keeping track of when flares happen.
Ongoing Use of Antifungal Shampoos
You’ll see the best results when you use medicated shampoos two to three times weekly on an ongoing basis. Ketoconazole and ciclopirox target the fungal infection that drives seborrheic dermatitis, reducing fungal density and keeping dandruff under control.
Rotating between different antidandruff formulas—like zinc pyrithione or selenium sulfide—promotes treatment adherence, protects scalp health, and may help prevent antifungal resistance over time.
Recognizing and Avoiding Triggers
Your seborrheic dermatitis is affected by more than just shampoos—it reacts to environmental humidity, stress management, and lifestyle changes you make daily. Cold, dry air worsens flaking, while tight hats trap moisture and aggravate this skin condition.
Dietary factors like omega-3 imbalances may influence the fungal infection driving your dandruff. Building trigger awareness helps you spot what sparks flare-ups before they take hold.
Tracking Flare Patterns
Consistent symptom logging reveals how your seborrheic dermatitis behaves over weeks to months, giving you control through pattern recognition.
Track flare cycles with:
- Weekly severity scores that capture itching and flaking intensity
- Trigger identification diaries linking stress, diet, and sleep to disease monitoring
- Seasonal observations showing when your scalp skin condition worsens
This dandruff tracking transforms guesswork into actionable dermatitis management.
When to Consult a Dermatologist
Most cases of seborrheic dermatitis respond well to over-the-counter treatments and consistent home care, but some situations call for professional guidance.
You shouldn’t try to push through severe symptoms or complications on your own, as a dermatologist can offer targeted solutions that aren’t available elsewhere.
Knowing when to seek expert help ensures you get the right treatment before the condition impacts your daily life or leads to secondary problems.
Persistent or Worsening Symptoms
If your scalp treatment isn’t working after four weeks, don’t brush it off—persistent symptoms or symptom escalation signal a need for professional evaluation. Chronic inflammation that worsens with over-the-counter care, especially when paired with scalp pain, fever management concerns, or signs of infection control issues, warrants immediate attention. Seborrheic dermatitis can mimic psoriasis or contact dermatitis, making accurate diagnosis essential.
| Warning Sign | When to Act |
|---|---|
| No improvement after 4 weeks | Schedule dermatology visit |
| Increased redness or crusting | Seek prompt evaluation |
| Severe scalp pain or fever | Contact provider immediately |
| Persistent flaking despite treatment | Consider differential diagnosis |
| Worsening dandruff symptoms | Rule out secondary infection |
Signs of Infection or Complications
Vigilance matters when treating seborrheic dermatitis because bacterial infections and fungal complications can quickly escalate. Watch for pus-filled lesions, increased redness beyond typical inflammation, or fever—these infection signs demand urgent skin infection treatment.
If you’re immunocompromised or notice painful swelling, lymph node enlargement, or scalp infections with warmth and discharge, contact your dermatologist immediately for proper skin condition management and immune system disorders evaluation.
Personalized Treatment Planning
Your dermatologist designs personalized regimens by analyzing your unique patient profile—scalp severity, response history, and lifestyle constraints all shape your path forward.
Personal health management for seborrheic dermatitis succeeds when therapy adjustments respond to real-world symptom tracking:
- Shampoo frequency adjusted to individual flare patterns
- Combination treatments matched to adherence capability
- Objective measures guiding ongoing therapy adjustments
- Follow-up schedules ensuring ideal treatment outcomes
Frequently Asked Questions (FAQs)
Can diet changes help reduce seborrheic dermatitis?
Diet may modestly influence skin health, though evidence remains mixed. Some people notice improvement reducing inflammatory foods or boosting omega-3 intake, but dietary changes should complement—not replace—dermatology-recommended treatments for managing seborrheic dermatitis effectively.
When evaluating the effectiveness of treatments, it’s vital to verify scientific study summaries for accurate assessments.
Is seborrheic dermatitis contagious to other people?
You can’t pass seborrheic dermatitis to others through skin contact. Public health authorities don’t classify it as contagious, so no isolation or special precautions are needed around family or friends.
Does seborrheic dermatitis cause permanent hair loss?
Good news: seborrheic dermatitis won’t permanently rob you of your hair.
Scalp inflammation stays superficial, sparing follicles from destruction.
Once you control the flaking and redness, normal hair cycling bounces back.
Can stress alone trigger a seborrheic dermatitis flare?
Stress triggers can worsen seborrheic dermatitis flare symptoms by compromising your skin barrier and amplifying inflammation response, though it rarely acts alone—fungal infection and other factors usually contribute to dandruff outbreaks alongside stress.
Are natural remedies effective for seborrheic dermatitis?
Natural remedies like tea tree oil show antifungal activity against Malassezia, yet they don’t match prescription antifungals in clinical trials.
They work best as supportive additions to proven treatments rather than standalone solutions.
Conclusion
Picture your scalp calm, balanced, and finally free from that relentless cycle of flaking and irritation.
Effective seborrheic dermatitis dandruff treatment isn’t about quick fixes—it’s about understanding what drives your inflammation and selecting the right combination of antifungal agents, careful cleansing habits, and trigger avoidance.
With consistent management and attention to your skin’s signals, you can maintain long-term control and prevent those frustrating flares from dictating your daily comfort.
- https://academichelpexpress.blog/2024/08/please-use-the-bulleted-points-and-the-rubric-below-to-guide-your-work-your-pa/
- https://x.com/godofprompt/status/1990526288063324577
- https://www.sciencedirect.com/science/article/pii/S0749208123000268
- https://www.linkedin.com/posts/bohdanlukianets_tasks-study-research-activity-7373377539521667072-UTEi
- https://arxiv.org/html/2507.17948v2