This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.
Your scalp shouldn’t feel like a battleground, but seborrheic dermatitis scalp care often becomes a daily struggle against stubborn flakes and relentless itch. This chronic inflammatory condition affects nearly 5% of adults, triggered by an overgrowth of yeast that lives naturally on your skin.
Unlike simple dandruff, seborrheic dermatitis creates greasy, yellowish scales and patches of redness that resist ordinary shampoos. The condition flares unpredictably, worsening with stress, cold weather, or harsh hair products that strip your scalp’s protective barrier.
Managing it requires more than wishful thinking—you need targeted treatments, gentle daily care habits, and an understanding of what sets your scalp off.
Table Of Contents
- Key Takeaways
- What is Seborrheic Dermatitis of The Scalp?
- Key Causes of Scalp Seborrheic Dermatitis
- Recognizing Scalp Symptoms and Flare-Ups
- Diagnosing Seborrheic Dermatitis on The Scalp
- Everyday Scalp Care Tips
- Medicated Shampoo and Topical Treatments
- Natural Remedies and Home Care
- Lifestyle Changes to Prevent Flare-Ups
- Managing Severe or Persistent Cases
- Tips for Healthy Hair With Seborrheic Dermatitis
- Frequently Asked Questions (FAQs)
- Conclusion
Key Takeaways
- Seborrheic dermatitis creates greasy, yellowish scales driven by Malassezia yeast overgrowth and skin barrier breakdown, requiring targeted antifungal treatments rather than standard dandruff products.
- Medicated shampoos with ketoconazole, selenium sulfide, or zinc pyrithione form the treatment backbone, often combined with short-term topical steroids for faster inflammation control.
- Daily scalp care with lukewarm water, gentle fingertip massage, and sulfate-free pH-balanced shampoos prevents buildup and protects your compromised skin barrier without triggering flare-ups.
- Stress management, avoiding temperature extremes, and rotating treatment ingredients prevent resistance while maintaining long-term symptom control in this chronic condition.
What is Seborrheic Dermatitis of The Scalp?
Seborrheic dermatitis is a common skin condition that causes red, flaky patches on your scalp. It’s related to an overgrowth of yeast that naturally lives on your skin.
Let’s look at what you might notice if you have this condition.
Common Symptoms
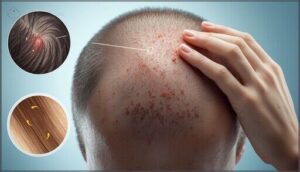
Scalp itching often announces seborrheic dermatitis before you notice anything else. You’ll see flaky skin that ranges from white to yellowish scales scattered across your scalp. Redness symptoms appear beneath these patches, creating skin irritation that won’t quit.
The itchy patches may feel greasy rather than dry, setting this condition apart from simple dandruff. Some people experience soreness or burning alongside the persistent itch.
If you’re wondering why your scalp feels sore or tender, inflammation from seborrheic dermatitis could be the underlying cause.
Areas Commonly Affected
You might notice scalp symptoms in predictable zones. The center of your head, temples, and behind your ears show the most activity. Here’s where seborrheic dermatitis commonly strikes:
These patches often look like raised, flaky areas that differ from regular dandruff, with thicker scales and more pronounced redness.
- Your scalp vertex and forehead develop scaling due to concentrated oil glands
- Eyebrows and nasolabial folds produce facial rashes and skin lesions
- The ear canal area becomes vulnerable to irritation
Men often see itchy skin spread to their beard region.
How It Differs From Dandruff
Understanding the clinical boundary between these scalp conditions helps you recognize what you’re dealing with. Dandruff symptoms involve dry, fine flakes that brush off easily without much redness. Seborrheic dermatitis brings thicker, oily scales that stick to your hair and come with noticeable skin inflammation.
| Feature | Dandruff | Seborrheic Dermatitis |
|---|---|---|
| Scale Type | Dry, powdery | Greasy, yellowish |
| Redness | Minimal | Pronounced erythema |
| Pattern | Diffuse flaking | Patches with adherent scales |
The fungal causes overlap, but dermatitis types produce more persistent itchy scalp symptoms requiring targeted treatment beyond cosmetic care.
Choosing the right products for itchy scalp can make a significant difference in managing seborrheic dermatitis and related conditions.
Key Causes of Scalp Seborrheic Dermatitis
Seborrheic dermatitis doesn’t have one simple cause. Instead, several factors work together to trigger symptoms on your scalp.
Understanding what’s happening beneath the surface helps you take control of flare-ups and find relief.
Role of Malassezia Yeast
A yeast infection drives much of what you experience with seborrheic dermatitis. Malassezia—a yeast that lives on everyone’s skin microbiome—feeds on scalp oils through lipid metabolism, creating fatty acids that trigger an immune response. This fungal infection causes the scaling, redness, and irritation you see.
When Malassezia overgrows in oily areas, your skin reacts, leading to persistent scalp scaling and discomfort.
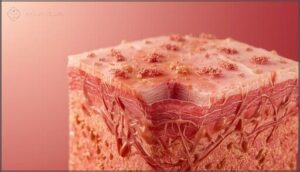
Skin Barrier Dysfunction
Beyond the yeast overgrowth, your skin’s protective wall plays a critical role. Barrier repair becomes essential when seborrheic dermatitis disrupts the stratum corneum—your scalp’s outermost defense. This breakdown allows irritants to penetrate deeper, triggering your immune system and worsening scalp scaling.
Three key changes compromise skin health:
Choosing a quality beard oil with natural ingredients helps restore balance by nourishing both skin and hair without synthetic additives that strip away protective oils.
- Altered ceramide therapy needs from lipid imbalance
- Increased water loss through damaged barriers
- Disrupted skin pH regulation affecting protective function
Genetic and Environmental Factors
Your genetic blueprint sets the stage, but environmental triggers flip the switch. Family history raises your risk two to three times, with polygenic factors shaping sebum production and immune system responses. Cold weather, harsh products, and stress heighten yeast interaction at the skin barrier. Gene expression shifts under environmental pressure—oxidative stress meets susceptible pathways, disrupting skin health and fueling seborrheic dermatitis flare-ups.
| Genetic Factors | Environmental Triggers | Combined Impact |
|---|---|---|
| Family history doubles risk | Winter cold worsens symptoms | Barrier breakdown accelerates |
| Twin concordance observed | Harsh cosmetics irritate scalp | Malassezia overgrowth increases |
| HLA haplotype variants linked | Urban pollution exposure | Inflammation intensifies |
| Polygenic risk pattern | Occupational humidity | Flare-up frequency rises |
Recognizing Scalp Symptoms and Flare-Ups
Recognizing the signs of seborrheic dermatitis on your scalp helps you catch flare-ups early and take action.
The symptoms can vary from person to person, but certain patterns appear consistently. Let’s look at the key signs you’ll want to watch for.
Types of Flaking and Scaling
You’ll notice scalp flaking in seborrheic dermatitis doesn’t look like typical dandruff. The scales are often yellowish and greasy, coating your hair shafts with an oily texture that requires careful sebum control.
Sometimes you’ll see fine white flakes mixed with red patches. These scales cluster along your hairline and behind your ears, creating visible scalp buildup that standard flake removal methods won’t easily clear.
Itchiness and Discomfort
Scalp itchiness affects 50 to 80 percent of people with seborrheic dermatitis symptoms, often peaking during evening hours or after sweating. The inflammatory response triggers nerve endings, creating a persistent itch-scratch cycle that worsens dandruff and irritation.
Common sources of scalp sensitivity and discomfort include:
- Burning or stinging sensations alongside pruritus management challenges
- Tight, uncomfortable scalp texture from inflammatory response
- Sleep disruption due to nocturnal itchy scalp episodes
- Heat and friction from headwear aggravating scalp irritation
- Stress-related flare-up triggers intensifying discomfort relief needs
Redness and Lesion Patterns
Erythema patterns in seborrheic dermatitis appear as light pink to deep red patches, often with irregular borders and greasy scales. Redness intensity varies based on your skin type and inflammatory response level.
Lesion distribution usually concentrates along the hairline and vertex, with flare triggers like cold weather or stress worsening scalp inflammation.
This skin condition requires targeted dermatitis treatment for symptom control.
Diagnosing Seborrheic Dermatitis on The Scalp
Getting the right diagnosis is your first step toward real relief. Your doctor will look at your scalp closely and rule out other conditions that might look similar.
Let’s walk through what happens during a diagnostic visit and when it’s time to see a specialist.
Physical Examination
During a physical examination, your dermatologist carefully inspects your scalp for greasy, white-yellow flaking and well-defined red patches. These examination techniques help distinguish seborrheic dermatitis symptoms from other scalp conditions through skin lesions characteristics. Your medical history also guides the diagnostic process.
- Waxy scales usually cluster around hair follicles and behind ears
- Bilateral symmetry suggests seborrheic dermatitis rather than infection
- Absence of pustules helps rule out bacterial scalp issues
Differential Diagnosis
Your dermatologist compares your symptoms against other dermatological conditions to confirm seborrheic dermatitis. Fungal infections like tinea capitis require fungal testing or skin biopsy to identify. Psoriasis shows thicker silvery scales and nail changes. Contact dermatitis links to specific allergen exposure. Immune system disorders may cause similar flaking.
These diagnostic criteria help rule out scalp infections and guarantee you receive targeted treatment for your actual dermatitis.
When to See a Dermatologist
Once you’ve ruled out other conditions, knowing when to seek medical evaluation helps you avoid complications. You need a dermatologist referral if over-the-counter treatments fail after four to six weeks. Watch for these signs requiring urgent care:
- New oozing, crusting, or signs of skin infection
- Severe redness spreading rapidly with pain or fever
- Persistent seborrheic dermatitis symptoms despite appropriate therapy
- Scalp assessment concerns in children or immunocompromised patients
Early dermatitis treatment prevents worsening.
Everyday Scalp Care Tips
Taking care of your scalp every day can reduce flare-ups and keep symptoms under control. The right approach starts with how you wash your hair and what products you use.
Here’s what works best for managing seborrheic dermatitis at home.
Gentle Cleansing Techniques
You’ll want to wash your scalp two to three times a week using lukewarm water, which helps control oil without triggering irritation. Start with a pre-rinse to soften any scales before applying product.
When you lather, use your fingertips in small circular motions—this scalp massage improves circulation and loosens flakes gently. Avoid scratching or scrubbing hard, as that weakens your skin barrier and worsens seborrheic dermatitis.
Rinse thoroughly to prevent buildup that can fuel dandruff. Pat your scalp dry instead of rubbing it. These cleansing routines protect sensitive skin while keeping your scalp care effective and comfortable.
Choosing Mild Shampoos
Once you’ve got your cleansing technique down, the right shampoo makes all the difference. Look for gentle formulas that calm rather than aggravate your scalp. Here’s what to prioritize in scalp care:
- pH-balanced options around 5.5 support your skin barrier and cut irritation.
- Sulfate-free shampoos strip fewer natural oils from sensitive scalps.
- Fragrance options matter—unscented choices reduce allergy risk.
- Scalp soothers like aloe or chamomile offer comfort during flare-ups.
- Medicated shampoos can complement mild products for dandruff treatment.
Check shampoo ingredients carefully. Noncomedogenic formulas won’t clog pores or worsen inflammation.
Medicated Shampoo and Topical Treatments
Medicated shampoos and topical treatments form the backbone of seborrheic dermatitis management. You’ll find options ranging from drugstore shelves to prescription-only formulas, each targeting the yeast and inflammation that drive your symptoms.
Let’s break down what’s available and how these treatments work to bring your scalp back under control.
Over-the-Counter Options
You’ll find several effective OTC treatments at your local pharmacy. Antifungal shampoos with ketoconazole or selenium sulfide target yeast directly. Zinc pyrithione shampoos offer antimicrobial benefits, while coal tar formulas reduce scaling. Salicylic acid-based gentle cleansers loosen flakes but can dry your scalp, so pair them with conditioner. Ultra-low strength topical corticosteroid solutions provide temporary relief from itching and inflammation.
For accurate diagnosis and treatment, it’s vital to apply scientific study methods to secure the best outcomes.
Prescription-Strength Shampoos
When OTC options don’t clear your scalp, your dermatologist may prescribe higher-strength formulas. Prescription-strength shampoos contain concentrated ketoconazole, selenium sulfide, or pyrithione zinc that penetrate deeper into affected skin. Treatment duration usually spans several weeks.
Your clinician will discuss medication interactions, potential side effects, and prescription costs. Follow dosing instructions carefully, and report any worsening symptoms during scalp therapy.
To better understand complex medical terms, you can search for language definitions and find related words.
Antifungal and Steroid Solutions
Antifungal therapy targets the Malassezia yeast that fuels seborrheic dermatitis on your scalp. Ketoconazole and ciclopirox are common antifungal agents in medicated shampoos.
Steroid creams calm inflammation quickly, but you’ll use them for short bursts to avoid skin thinning.
Many clinicians pair antifungal shampoos with low-potency steroids for faster relief. This combination approach tackles both fungal infections and uncomfortable flare-ups while maintaining medication safety.
Natural Remedies and Home Care
Many people with seborrheic dermatitis turn to natural options alongside medical treatments. These home remedies can help calm irritation and support your scalp’s healing process.
Let’s look at some gentle, evidence-based approaches you can try at home.
Soothing Oils and Ingredients
You can turn to natural remedies for gentle scalp care tips. Tea tree oil fights the Malassezia yeast when diluted properly, while coconut oil delivers antifungal benefits through lauric acid. Aloe vera gel calms redness and itching on contact.
Jojoba and argan oils moisturize without clogging follicles. Oil blending helps you target dryness and inflammation. These essential oil benefits support natural hair care routines effectively.
Scalp Massage Benefits
Gentle massage techniques give your scalp more than just relaxation therapy—they improve blood flow and itch relief while helping treatments work better. Regular scalp care tips like these address scalp buildup and support overall scalp health in seborrheic dermatitis.
Massage frequency matters for lasting comfort.
- Boost circulation by 15% with moderate pressure during massage
- Cut itch intensity by 20–30% within 10 minutes
- Lower stress markers like cortisol through relaxing touch
- Spread treatments evenly across your scalp for better absorption
Safe Use of DIY Treatments
Homemade remedies can backfire if you skip basic DIY precautions. Essential oil safety starts with dilution—undiluted oils trigger scalp irritation in 5–10% of users. Patch test natural ingredients first, limit use to 1–2 weeks, and avoid mixing multiple DIY treatments without guidance. Keep tools sterile to prevent infections.
For seborrheic dermatitis on your scalp, natural remedies work best alongside medicated shampoos.
Lifestyle Changes to Prevent Flare-Ups
Your daily habits can make a real difference in how often flare-ups happen. Simple changes to your routine help strengthen your skin’s natural defenses and keep yeast growth in check.
Here’s what you can adjust to take control of your scalp health.
Managing Stress Levels
Stress response directly affects your immune system and scalp health, often triggering seborrheic dermatitis flare-ups. Mindful relaxation through meditation benefits your emotional wellness while potentially reducing symptoms by 20-30%.
Try simple relaxation techniques like deep breathing or progressive muscle relaxation for 10-15 minutes daily. Regular aerobic exercise and seven to nine hours of quality sleep also lower inflammation naturally.
Diet and Hydration for Skin Health
What you eat directly nourishes your skin barrier and scalp health. Nutrient balance matters—omega fatty acids reduce inflammation while antioxidant-rich foods like berries and leafy greens lower oxidative stress linked to seborrheic dermatitis flare-ups.
Skin hydration improves when you drink enough water throughout the day, and adequate electrolyte intake helps maintain moisture balance.
Avoiding high-sugar meals can reduce excess sebum production that worsens symptoms.
Avoiding Common Triggers
Beyond what you eat, managing environmental factors helps keep seborrheic dermatitis symptoms under control. Humidity control and yeast management matter—excessive moisture encourages Malassezia growth on your scalp. Irritant minimization means skipping harsh detergents that weaken your skin barrier.
Temperature extremes, seasonal shifts, and alcohol-based products can trigger flare-ups. Protecting your scalp’s skin pH through trigger avoidance reduces dandruff and inflammation.
Managing Severe or Persistent Cases
When your scalp doesn’t respond to standard treatments, you may need more specialized care. Severe or persistent seborrheic dermatitis requires a step-up approach that goes beyond everyday shampoos and home remedies.
Here’s what to keep in mind when your symptoms refuse to settle down.
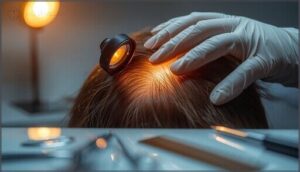
When to Consider Phototherapy
When standard topical treatments for seborrheic dermatitis on your scalp don’t work after months of consistent use, phototherapy benefits may offer relief. Dermatology experts use UVB treatment for refractory cases with widespread or persistent symptoms.
This skin condition treatment helps control flare-ups, though you’ll need monitoring for skin irritation or photo damage risks. Seborrheic dermatitis treatment plans are individualized based on your severity and skin type.
Long-Term Treatment Strategies
Successful treatment of seborrheic dermatitis often requires rotating medicated shampoos with different active ingredients—like ketoconazole, selenium sulfide, or zinc pyrithione—to prevent resistance and maintain scalp health.
Your dermatologist may recommend combination therapy for stubborn cases, pairing antifungal shampoos with low-dose topical steroids or calcineurin inhibitors.
Consistent medication management and regular follow-ups help fine-tune treatment outcomes while minimizing side effects and preventing scalp buildup.
Monitoring for Complications
Vigilance in tracking your scalp health helps catch complications early and keeps your dermatitis treatment on course. Watch for these warning signs:
- Crusting or oozing lesions may signal a secondary bacterial infection requiring prompt care.
- Worsening redness or pain can indicate treatment failure or resistant organisms.
- Persistent flaking beyond several weeks suggests your current regimen needs adjustment.
- New pustules or folliculitis warrant immediate dermatologist evaluation.
- Sleep disruption from itching affects quality of life and needs addressing.
Tips for Healthy Hair With Seborrheic Dermatitis
Managing seborrheic dermatitis doesn’t mean you have to compromise your hair’s health. You can maintain strong, beautiful hair while treating your scalp condition.
Here’s how to protect your hair and support its natural growth.
Minimizing Hair Damage
When seborrheic dermatitis flares, your scalp becomes more vulnerable to hair breakage. Gentle shampooing with medicated shampoos protects your scalp while minimizing damage.
Pat hair dry instead of rubbing vigorously. Use a wide-tooth comb for detangling and apply hair conditioning treatments to mid-lengths and ends.
Proper hair care during treatment aids damage prevention and healthy hair growth despite ongoing scalp challenges.
Safe Styling Practices
Think of your scalp like wounded skin—it needs rest from tension and trauma. Choose hairstyles that don’t pull or tug. Avoid tight ponytails and braids that worsen seborrheic dermatitis.
Skip heat tools when possible, as they stress your scalp further. Use gentle products free from harsh chemicals and fragrances. Before trying new styling aids, do a patch test to protect your scalp health.
Supporting Hair Growth and Strength
Healthy hair starts at the follicle, and controlling inflammation directly aids hair follicle health. Here’s how you can strengthen your hair while managing seborrheic dermatitis:
- Use medicated shampoos regularly to reduce yeast and support sebum regulation, creating stable conditions for hair growth.
- Try gentle scalp massage to boost blood flow without aggravating symptoms, enhancing scalp health.
- Practice gentle hair care—skip harsh chemicals that compromise hair shaft integrity and increase breakage.
Frequently Asked Questions (FAQs)
Can seborrheic dermatitis cause permanent hair loss?
Most people notice their hair returns once inflammation settles. Permanent follicle damage isn’t typical with seborrheic dermatitis, though temporary shedding from scalp inflammation can worry you until effective dermatitis treatment restores normal hair growth.
Is seborrheic dermatitis contagious to other people?
No, you can’t spread this condition to others. The Malassezia yeast involved already lives on everyone’s skin, so there’s no contagion risk through contact or shared items.
How long do typical flare-ups usually last?
Flare duration varies by treatment response and trigger factors. Most episodes last several days to a few weeks with medicated shampoo, while untreated scalp buildup may persist two to six weeks before natural remission periods begin.
Can children develop seborrheic dermatitis on scalp?
Yes, seborrheic dermatitis strikes young scalps too. Infants often show cradle cap with yellowish crusts, while older children may develop scalp scaling.
Pediatric scalp care focuses on gentle cleansing and addressing youthful scalp symptoms early.
Does seborrheic dermatitis ever go away completely?
Seborrheic dermatitis usually persists as a chronic condition with remission periods and flare-ups rather than a complete cure.
Long-term management strategies help control symptoms and extend remission, but symptom relapse remains common even with treatment.
Conclusion
Your scalp’s story doesn’t end with a diagnosis—it evolves with every choice you make. Effective seborrheic dermatitis scalp care means finding what calms your inflammation, whether that’s medicated shampoos, stress management, or avoiding triggers.
Flare-ups won’t vanish overnight, but consistent attention shifts the balance in your favor. You’ve learned to recognize symptoms, select treatments, and protect your skin‘s barrier.
That knowledge becomes your greatest tool for reclaiming comfort and confidence, one wash at a time.